Understanding Bertolotti Syndrome
Introduction to the Condition
Bertolotti’s Syndrome is a congenital condition affecting the lumbar spine, causing chronic lower back pain due to a lumbosacral transitional vertebra (LSTV) – a condition where the lowest lumbar vertebra partially or fully fuses with the sacrum. Bertolotti’s Syndrome is defined as a pain syndrome associated with lumbosacral transitional vertebrae, characterized by chronic lower back pain linked to this anatomical anomaly.
Many individuals with an LSTV are asymptomatic, and only those with symptomatic lumbosacral transitional vertebrae develop Bertolotti’s Syndrome. Symptoms may not appear until adulthood, with numerous clinical manifestations leading to delayed diagnosis.
This fusion disrupts the normal weight distribution across the pelvis, leading to chronic pain and reduced mobility in the lower back. Unilateral or bilateral enlargement of the transverse process is a key radiological feature of the condition.
The clinical significance of Bertolotti’s Syndrome lies in its role as a potential cause of chronic lower back pain, impacting diagnosis, treatment decisions, and patient outcomes. The condition is characterized by sacroiliac joint pain, lumbar spine degeneration, and diagnostic and management dilemmas. More significant spinal degeneration can occur above the transitional vertebra.
Patients with Bertolotti’s Syndrome often experience chronic low back pain, which can be challenging to manage.
Bertolotti syndrome is named after the Italian scientist who discovered it in 1917.
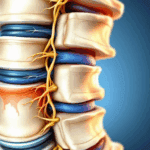
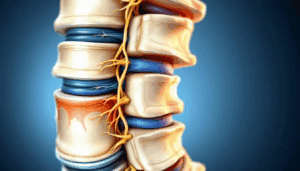
Anatomy of the Lumbar Spine
The lumbar spine forms the foundation of the lower back, consisting of five robust vertebrae labeled L1 through L5. These vertebrae are designed to support much of the body’s weight while allowing for flexibility and movement. Key components of the lumbar spine include the vertebral bodies, which bear weight; the intervertebral discs, which cushion and absorb shock; and the facet joints, which guide motion and provide stability. The spinous and transverse processes serve as attachment points for muscles and ligaments, contributing to the spine’s strength and flexibility.
In Bertolotti’s Syndrome, the anatomy of the lumbar spine is altered by the presence of a lumbosacral transitional vertebra (LSTV), where the lowest lumbar vertebra partially fuses with the sacrum. This abnormality can disrupt normal biomechanics, leading to chronic low back pain and sacroiliac joint pain. Understanding the unique structure of the lumbar spine is essential for diagnosing and managing Bertolotti’s Syndrome, as these anatomical changes are directly linked to the development of chronic pain and reduced mobility in affected individuals.
Causes and Pathophysiology
- The exact cause of Bertolotti’s Syndrome is unclear, but it is believed to be related to genetic factors and abnormal spinal development.
- The most caudal vertebra, typically L5, fuses with the sacrum or ilium in Bertolotti syndrome.
- The condition alters the normal biomechanics of the lumbar spine, leading to hypomobility at the L5-S1 level and hypermobility above, resulting in degenerative changes and pain. In normal skeletal anatomy, the sacrum’s size, surface area, and sacroiliac joint are utilized to dissipate upper body weight across the fused sacrum into the legs, maintaining spinal biomechanics. In Bertolotti’s Syndrome, this normal weight distribution is disrupted, increasing stress on adjacent segments.
- The sacroiliac joint dysfunction association is a significant factor in the development of chronic pain in patients with Bertolotti’s Syndrome.
- The condition can lead to premature disc degeneration due to increased stress on the L4-L5 disc and facet joints. Disc herniation is a common consequence of these altered biomechanics in patients with Bertolotti’s Syndrome. Acute lumbar disc herniation can also occur at a younger age in patients with lumbosacral transitional vertebrae (LSTV).
- The condition can lead to numerous clinical manifestations, including radicular pain, degenerative spine changes, and significant spinal degeneration. In addition to ipsilateral facet joint pain, contralateral facet joint pain may also develop due to altered load distribution. These anatomical and biomechanical changes can result in chronic pain caused by the transitional vertebra.
Symptoms and Diagnosis
- Patients with Bertolotti’s Syndrome typically report chronic lower back pain, which can be accompanied by radicular pain, numbness, and tingling sensations in the legs. It is crucial to identify the specific generator of the patient’s pain, such as whether it is discogenic, facet joint-related, or due to pseudoarticulation, to guide effective diagnosis and management.
- Symptoms of Bertolotti syndrome can include unilateral low back pain, pain radiating to the hips, groin, and buttocks, stiffness, and reduced range of motion. Many patients report daily pain that significantly impacts their quality of life.
- The diagnosis of Bertolotti’s Syndrome involves a combination of clinical assessment, imaging studies (X-rays, CT, and MRI), and selective nerve root blocks to confirm the presence of an LSTV and related degenerative changes. Pain patients with Bertolotti’s Syndrome require thorough evaluation to determine the source and nature of their symptoms.
- The pain disability questionnaire and vas pain quantifying system can be used to assess pain and disability levels in patients with Bertolotti’s Syndrome.
- A thorough clinical evaluation is essential to rule out other potential causes of chronic lower back pain. Pain management arose from the need to address the complex and varied pain presentations in these patients.
Treatment and Management
- The management of Bertolotti’s Syndrome requires a multidisciplinary approach, including conservative treatment options, such as physical therapy, steroid injections, and pain management. Physical therapy represents a cornerstone of non-surgical management.
- Patients undergoing manual therapy, such as lumbosacral manipulation and physiotherapy, may experience improved mobility and pain reduction.
- Pain from Bertolotti syndrome may worsen with extension or prolonged sitting and improve when lying down. Both nociceptive and mechanical pain can be addressed through targeted interventions.
- The goal of treatment is to relieve pain, improve function, and manage pain effectively, using a combination of non-surgical and surgical interventions. The importance of initial pain treated is significant in determining long-term outcomes.
- Pain physicians play a crucial role in the management of Bertolotti’s Syndrome, using a range of treatment options, including injection therapy and surgical intervention. Steroid injection is a commonly used intervention for inflammation and pain. General sacroiliac joint pain may also be managed with these approaches. When procedural pain compared across interventions, some techniques may offer reduced discomfort for patients.
Conservative Treatment Options
- Conservative treatment options for Bertolotti’s Syndrome include physical therapy, steroid injections, and pain management.
- Minimal physical exercise alone is generally less effective than structured interventions such as Pilates or manual therapy.
- Patients may undergo interlaminar epidural steroid injections to relieve nerve root symptoms and reduce pain.
- The use of steroid and anesthetic injections can provide relative pain relief lasting several months.
- Bertolotti syndrome causes an increased incidence of disc herniations and facet arthrosis at levels above the transitional vertebra. Discogenic pain involves introducing novel therapies such as RF lesioning and thermal resistive coils to target disc tissue and alleviate pain.
- Patients undergoing resection may experience complete pain control, but this is not always the case.
Response to conservative treatments, particularly anesthetic injections, may help predict future successful surgical management.
Surgical Intervention
- Surgical intervention may be necessary for patients with Bertolotti’s Syndrome who have failed previous lines of conservative treatment.
- Surgical procedures, such as surgical resection and spinal fusion, can provide positive pain relief and improve function. A range of surgical treatments is available for Bertolotti’s Syndrome, each with specific indications and potential risks.
- Some patients undergo decompression to relieve nerve impingement, which may be necessary to address radicular pain and improve mobility.
- Delayed treatment for Bertolotti syndrome can lead to worse physical and mental health outcomes.
- The surgical procedure should be tailored to the individual patient’s needs, taking into account the extent of degenerative changes and the patient’s overall health. Examining surgical efficacy compared to non-surgical options is important to determine the best approach for each patient.
- Successful surgical intervention can lead to significant pain relief and improved function.
Advanced Surgical Procedures
- Advanced surgical procedures, such as minimally invasive surgery, may be used to treat Bertolotti’s Syndrome. Studies published in Int J Spine Surg support advanced surgical approaches, including resection or fusion, for symptomatic cases involving lumbosacral transitional vertebrae.
- The use of minimally invasive techniques can reduce procedural pain and improve recovery times. Findings from Korean J Pain highlight favorable outcomes and evidence-based benefits of these minimally invasive approaches in pain management for Bertolotti’s Syndrome.
- Patients undergoing surgical intervention should be carefully selected, and the potential risks and benefits of surgery should be carefully weighed.
- The condition primarily affects individuals in their twenties and early thirties.
- The goal of surgical intervention is to provide significant pain reduction and improve function, while minimizing the risk of complications. Immediate pain reduction is often observed following certain surgical interventions, serving as both a therapeutic benefit and a diagnostic indicator.
Alternative Therapies
For individuals living with Bertolotti’s Syndrome, alternative therapies can play a valuable role in managing chronic low back pain and improving quality of life. Approaches such as acupuncture, massage therapy, and chiropractic care may help reduce chronic pain, ease muscle tension, and enhance mobility. Physical therapy remains a cornerstone of alternative management, focusing on gentle exercises and manual techniques to strengthen the lumbar spine and support pain relief.
Steroid injections are sometimes used alongside alternative therapies to address nerve root symptoms and provide targeted pain management. Additionally, practices like Pilates and yoga can improve flexibility and core strength, offering further relief for chronic low back pain. While some patients report positive outcomes with these therapies, it’s important to note that more research is needed to confirm their effectiveness specifically for Bertolotti’s Syndrome. Patients should consult with their healthcare provider to determine which alternative therapies may best complement their overall pain management plan.
Lifestyle Modifications
Making thoughtful lifestyle modifications is a key strategy in managing Bertolotti’s Syndrome and reducing chronic pain. Maintaining a healthy weight helps decrease stress on the lumbar spine, while regular, low-impact exercise—such as walking, swimming, or stretching—can improve flexibility and support pain relief. Practicing good posture throughout daily activities and avoiding heavy lifting, bending, or twisting can further protect the lower back and minimize sacroiliac joint pain.
Other important lifestyle changes include quitting smoking, which can slow degenerative spine changes, and managing stress, as chronic pain can be exacerbated by anxiety and tension. A balanced diet rich in anti-inflammatory foods supports healing and overall well-being. Patient education and support are essential, empowering individuals to make informed choices and actively participate in their care. By adopting these lifestyle modifications, patients can experience meaningful improvements in chronic low back pain and overall function.
Complications and Risks
If Bertolotti’s Syndrome is not properly managed, several complications and risks may arise. Chronic low back pain can lead to decreased mobility, limiting daily activities and negatively impacting mental health. Surgical treatment and other surgical interventions, while sometimes necessary, carry inherent risks such as infection, bleeding, and potential nerve damage. Additionally, patients may develop sacroiliac joint dysfunction or experience degenerative spine changes, which can further complicate pain management.
Nerve root symptoms, including radicular pain that radiates down the leg, are also possible complications. Over time, adjacent spinal segments may undergo increased wear and tear, leading to further degenerative changes. To address these risks, pain management strategies such as steroid injections and targeted therapies are often employed to control symptoms and prevent progression. Early intervention and a comprehensive treatment plan are crucial to minimizing complications and maintaining quality of life.
Exploring Treatment Options
- Lower back pain patients with Bertolotti’s Syndrome should explore all available treatment options, including conservative and surgical interventions.
- The use of injection therapy, including steroid and anesthetic injections, can provide pain relief and improve function. Relative pain relief lasting several months can be achieved with certain interventions.
- Patients often report daily pain above 5/10 in severity on average due to Bertolotti syndrome.
- Patients should work closely with their pain physician to develop a personalized treatment plan, taking into account their individual needs and goals.
- The treatment plan should be regularly reviewed and updated to ensure that the patient is receiving the most effective treatment possible.
Prognosis and Outcomes
- The prognosis for patients with Bertolotti’s Syndrome is generally good, with many patients experiencing significant pain reduction and improved function with treatment.
- However, the condition can be challenging to manage, and some patients may experience chronic back pain and disability that persists despite treatment.
- The incidence of Bertolotti syndrome is reported to be between 4% and 8% of the population, although it is considered underdiagnosed.
- The use of a multidisciplinary approach, including conservative and surgical interventions, can improve outcomes and reduce the risk of complications.
- Patients should work closely with their pain physician to develop a personalized treatment plan and regularly review and update their treatment plan to ensure the best possible outcomes.
Patient Education and Support
Empowering patients through education and support is fundamental to the successful management of Bertolotti’s Syndrome. Understanding the nature of chronic low back pain, available treatment options, and the importance of pain management enables patients to make informed decisions about their care. Education about the lumbar spine, sacroiliac joint pain, and the benefits of various therapies helps demystify the condition and fosters a proactive approach to health.
Support from a multidisciplinary team—including pain management specialists, physical therapists, and other healthcare professionals—ensures comprehensive care tailored to each patient’s needs. Participation in support groups or online communities can provide emotional encouragement and practical advice from others facing similar challenges. By prioritizing patient education and support, individuals with Bertolotti’s Syndrome can take an active role in managing their chronic pain, achieving pain relief, and improving their overall quality of life.
Enhancing Healthcare Team Outcomes
- The management of Bertolotti’s Syndrome requires a multidisciplinary approach, including pain physicians, physical therapists, and surgeons.
- The healthcare team should work closely together to develop a personalized treatment plan, taking into account the patient’s individual needs and goals.
- Common misdiagnoses for Bertolotti syndrome include sciatica and degenerative disc disease.
- The use of a team-based approach can improve outcomes and reduce the risk of complications.
- Patients should be encouraged to take an active role in their care, asking questions and seeking a second opinion if necessary.