Effective Tips for Fractured Vertebrae Recovery: Prevention and Treatment Insights
Recovering from a fractured vertebrae recovery can be challenging, but understanding the key steps can make a significant difference. In this article I will walk you through what to expect, treatment options, and practical tips for a smoother recovery. The risk of spinal fractures increases with age, particularly in adults over 50, making awareness and prevention crucial.
Key Takeaways
- Fractured vertebrae can result from conditions like osteoporosis or trauma, and prompt diagnosis is essential for effective treatment and recovery.
- Different types of vertebral fractures require tailored treatment plans, ranging from non-surgical methods like physical therapy to surgical interventions such as kyphoplasty.
- Long-term recovery involves active engagement in physical activities, regular follow-ups, and lifestyle adjustments to manage bone health and prevent future fractures. Most spinal fractures heal naturally over time within six to twelve weeks, emphasizing the importance of consistent care during this period.
Understanding Fractured Vertebrae

A fractured vertebra refers to a break occurring in any of the vertebrae in the spinal column. These fractures can result from various factors, including osteoporosis, trauma from falls or accidents, and certain health conditions. The spine is a complex structure made up of bones, or vertebrae, that protect the spinal cord and support the body’s weight, including a fractured bone. Females are more likely than males to experience spinal fractures due to factors such as osteoporosis and hormonal changes after menopause.
Common symptoms of fractured vertebrae include back pain, leg pain, numbness, and difficulty moving. These severe symptoms can significantly impact daily activities and quality of life, making prompt diagnosis and treatment essential. Initial diagnosis typically involves a physical examination and imaging tests like X-rays or CT scans. During the healing process, spinal bones heal in their new compressed shape, which can lead to height loss and a curved spine.
Recognizing the causes and symptoms of fractured vertebrae is crucial for effective treatment and recovery. Early identification allows for prompt medical attention and a swifter healing process.
Types of Vertebral Fractures
Vertebral fractures are categorized into different types, each with specific implications for recovery. One common type is the compression fracture, which often occurs due to weakened bones from conditions like osteoporosis. These fractures can take on a wedge shape when the front of the vertebra collapses.
Another type is the burst fracture, caused by significant forces that lead to multiple fractures in the vertebrae. This type of fracture can damage surrounding tissues, making it more severe. Flexion-distraction fractures result from sudden forward force, commonly occurring during abrupt stops or accidents like car crashes, which can lead to traumas.
Knowing the different types of vertebral fractures aids in determining the appropriate treatment and recovery plan. Each type presents unique challenges, necessitating a customized approach for effective healing.
Immediate Steps Post-Injury
Immediate medical evaluation is critical following a spinal injury, especially if there are neurological symptoms like numbness or difficulty walking. Prompt medical attention can prevent complications such as chronic pain or spinal deformities. Rest is essential to prevent worsening of pain and instability following a spinal injury, as it can help calm the nerves. Many spinal fractures can heal without the need for surgery, although some may require a brace for support.
Pain management often includes nonsteroidal anti-inflammatory drugs (NSAIDs) for effective relief. If severe pain occurs after a spinal fracture, rest and take pain-relieving medication. The initial steps taken post-injury can significantly impact the healing process and overall recovery. Pain relief medication does not assist in the healing process but may help you to remain mobile while your bones heal.
Following these immediate steps sets the foundation for a successful full recovery. Proper rest, effective pain management, and prompt medical attention are vital in the early stages to recover from a spinal injury.
Treatment Options for Fractured Vertebrae
Non-surgical treatments for spinal fractures include:
- Pain management
- Physical therapy, which can help rebuild muscle strength and coordination after a spine injury to treat spinal fractures. Spinal fractures treated with integrative health services, such as tai chi and meditation, are offered alongside traditional physical therapy to enhance overall recovery.
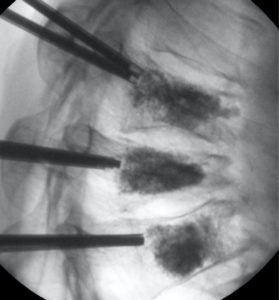
Surgical interventions like kyphoplasty and vertebroplasty are considered for more severe cases. Kyphoplasty involves the use of a balloon to restore vertebral height and stabilize the fracture with cement. Vertebroplasty, on the other hand, injects cement directly into the fractured vertebra to stabilize it without height restoration. Patients undergoing kyphoplasty often report significant pain relief shortly after the procedure.
The healing process for a spinal fracture typically spans six to twelve weeks, with ongoing activity being beneficial during recovery. Surgical intervention is typically considered for cases where non-surgical treatments fail or in the presence of severe pain.
Knowing the various treatment options helps patients and healthcare providers develop a tailored treatment plan. The aim, whether through non-surgical or surgical methods, is to stabilize the spine, manage pain, and heal naturally while promoting healing.
Pain Management Strategies
Medications such as over-the-counter anti-inflammatory medications like ibuprofen or stronger pain relievers may be prescribed for relief. Doctors typically prescribe pain medication for about two weeks post-injury to help manage discomfort. It is suggested to take pain relievers to help manage discomfort while trying to maintain mobility.
Non-pharmacological options for pain management include methods like transcutaneous electrical nerve stimulation and acupuncture. A reverse analgesia approach, starting treatment with strong opioids and reducing dosage as pain subsides, may be more effective for acute fracture pain. Home remedies such as using a hot water bottle or wheat bag can help relieve muscle spasms after a fracture.
Managing severe pain from vertebral fractures requires effective pain relief methods. Combining pharmaceutical and non-pharmaceutical approaches offers comprehensive pain management and enhances recovery outcomes, taking into account the pain level experienced by patients.
Role of Physical Therapy
Recommended exercises for recovery include:
- gentle movements
- walking
- water-based exercises
- pelvic tilts
- leg slides
- gentle core strengthening
Physical therapy is typically recommended later on, after the initial healing phase of a spine compression fracture. It is frequently recommended to strengthen the muscles supporting the spine, aiding in long-term recovery and reducing the risk of future injuries.
Should posture exercises cause significant pain, reduce repetitions or contraction length and consult your physiotherapist. Engaging in regular exercise and moderate-intensity exercise for at least 150 minutes weekly is crucial for maintaining overall bone health during recovery.
Using a Spinal Brace
A spinal brace is intended to restrict spinal movement, aiding healing and minimizing pain. The need for a spinal brace is determined by the type and location of the fracture, as well as other medical issues. The purpose of a back brace in treating compression fractures is to support and stabilize the spine during healing.
A back brace should be worn every day until the fracture heals, typically for about 8 weeks. Not all patients with spinal fractures need to wear a brace; this decision is based on individual circumstances. Weaning off the brace involves gradually reducing wear time over a period of 1 to 2 weeks. Stable spinal fractures do not push or pull the vertebrae out of alignment, whereas unstable fractures do, increasing the risk of serious complications.
While using a brace, patients are generally advised to avoid heavy lifting and twisting movements to prevent movement. Bracing off a spinal brace should be done gradually to ensure patient comfort and safety.
Potential Complications and Risks
Potential complications of a spinal fracture include nerve damage, infection, and chronic pain. Unstable spinal fractures are associated with a higher likelihood of serious complications compared to stable fractures. Patients may experience chronic pain from vertebral fractures due to ongoing degenerative changes around the fracture site.
Severe spinal fractures can lead to permanent damage to the spinal cord, potentially affecting mobility. Severe complications from spinal fractures can include nerve or spinal cord damage, paralysis, or even death. Potential damage to the spinal cord from severe spinal fractures might be permanent and irreversible.
In cases where surgery is necessary, there is a heightened risk for infections at the surgical site. Understanding these potential complications and risks can help patients who require surgery make informed decisions about their treatment and recovery plans.
Long-Term Recovery and Prevention

Individuals with a compression fracture are five times more likely to develop another fracture, highlighting the importance of bone health management. Avoiding bed rest minimizes the risk of blood clots or deep vein thrombosis. Regular physical therapy routines can significantly reduce the chances of further spine injuries.
Balance and coordination exercises may be included in physical therapy to diminish fall risks. Active participation in daily activities is encouraged to prevent complications such as chest infections and blood clots. Long-term recovery involves a combination of physical therapy, lifestyle adjustments, and proactive health management.
Returning to Daily Activities
Gradual re-engagement in activities is crucial, especially if severe pain occurs during initial exercises. Staying active reduces the risk of infections, constipation, and blood clots, while maintaining muscle strength. Low-impact exercises like swimming, cycling, and yoga are recommended for returning to activity after a spinal fracture. Listening to your body and pacing activity during recovery is important to avoid overexertion.
Avoiding high-impact activities after a spinal fracture is crucial to prevent further injury. Factors affecting the timing of returning to work after a fracture include the type of work, distance from home, and employer support. A phased return to work approach is recommended, gradually increasing hours and duties based on individual recovery.
Follow-Up Care
Follow-up visits allow healthcare providers to:
- Develop a tailored care plan based on the patient’s healing progress.
- Review X-rays during the follow-up appointments after a spinal fracture.
- Monitor the patient to prevent long-term complications from spinal fractures.
Patients often undergo physical evaluations to assess mobility and strength after a spinal injury at follow-up appointments, considering the severity of their condition. Regular adjustments may be necessary if the brace causes stress or discomfort, which would be addressed in follow-up care.
Most people have two follow-up appointments after a spinal fracture with their doctor. Follow-up care involves attending doctor’s appointments to monitor progress and address underlying causes like osteoporosis, ensuring a comprehensive approach to recovery.
Summary
Summarize key points from the blog post. Inspire the reader to take proactive steps in managing spinal health.
Frequently Asked Questions
What are the common causes of fractured vertebrae?
Fractured vertebrae commonly occur due to osteoporosis, trauma from falls or accidents, and specific health conditions. It is crucial to address these risk factors to prevent such injuries.
How are vertebral fractures diagnosed?
Vertebral fractures are diagnosed through a combination of physical examinations and imaging tests, primarily X-rays or CT scans. This approach ensures an accurate assessment of the injury.
What are the treatment options for spinal fractures?
Treatment options for spinal fractures typically include non-surgical methods like pain management and physical therapy, as well as surgical procedures such as kyphoplasty and vertebroplasty. It is essential to consult a healthcare professional to determine the most appropriate approach based on individual circumstances.
How can I manage pain from a spinal fracture?
To effectively manage pain from a spinal fracture, consider using medications alongside non-pharmacological methods, such as acupuncture, and home remedies like a hot water bottle. These approaches provide a comprehensive strategy for pain relief.
What should I expect during follow-up care?
During follow-up care, you should expect monitoring of healing progress, review of X-rays, physical evaluations, and potential adjustments to your treatment plan as necessary.