Understanding Foraminal Stenosis: Symptoms, Causes, and Treatments
Foraminal stenosis happens when the gaps in your spine tighten, putting pressure on nerves. The foraminal canal is the transitional bony canal that allows spinal nerves to pass from the spinal cord to other parts of the body. This can cause pain, tingling, and numbness, often in the neck and lower back. In this article, you’ll learn who is affected, the types and symptoms of foraminal stenosis, how it’s diagnosed, and the available treatments, both non-surgical and surgical.
Introduction to Foraminal Stenosis
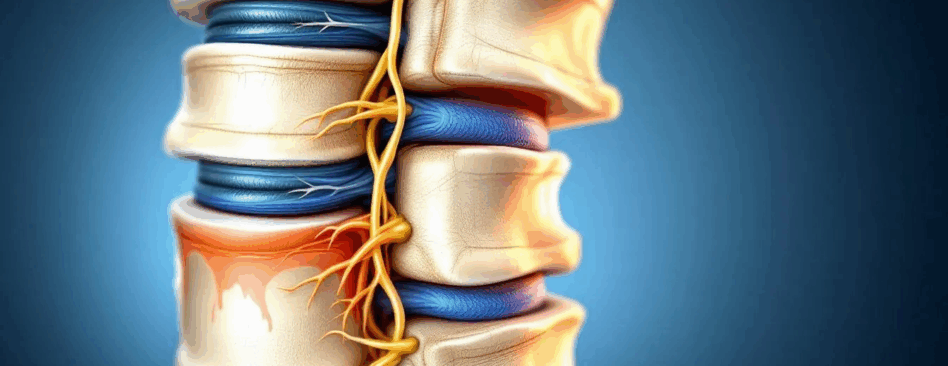
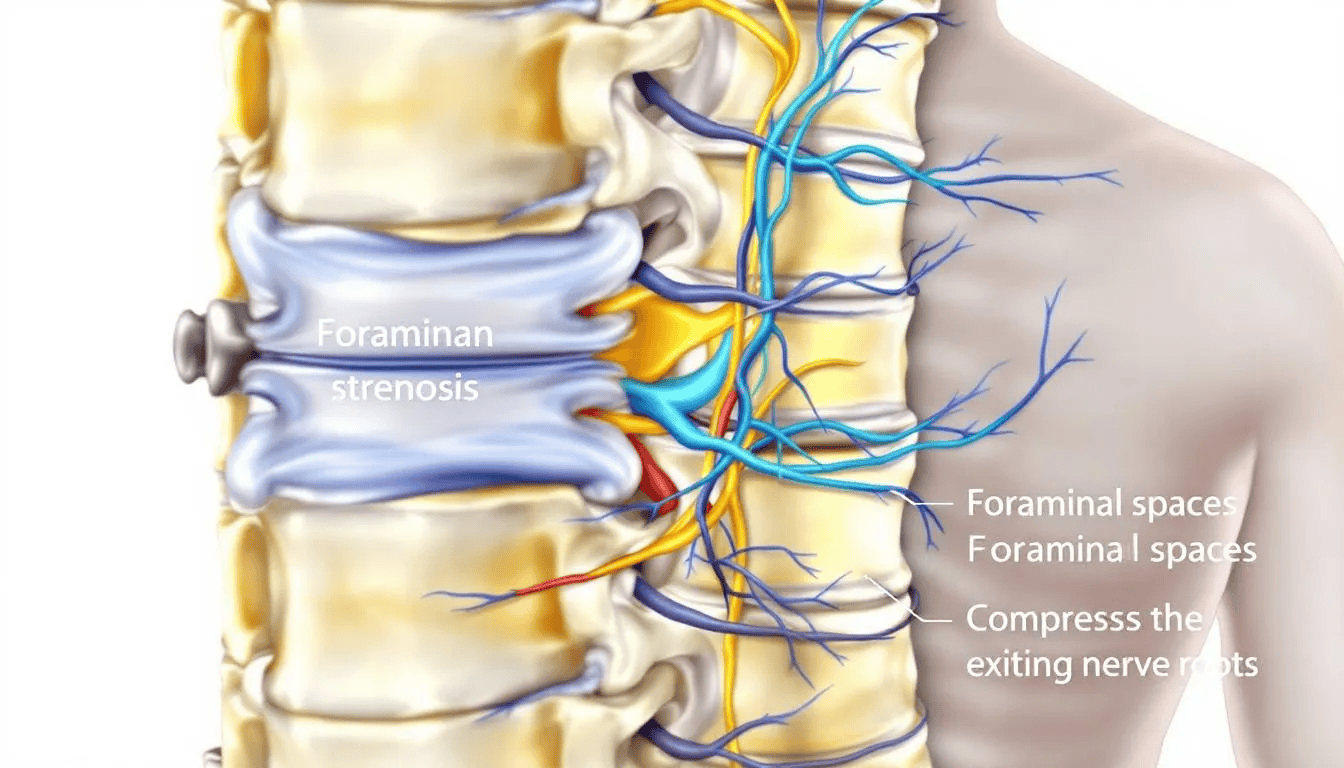
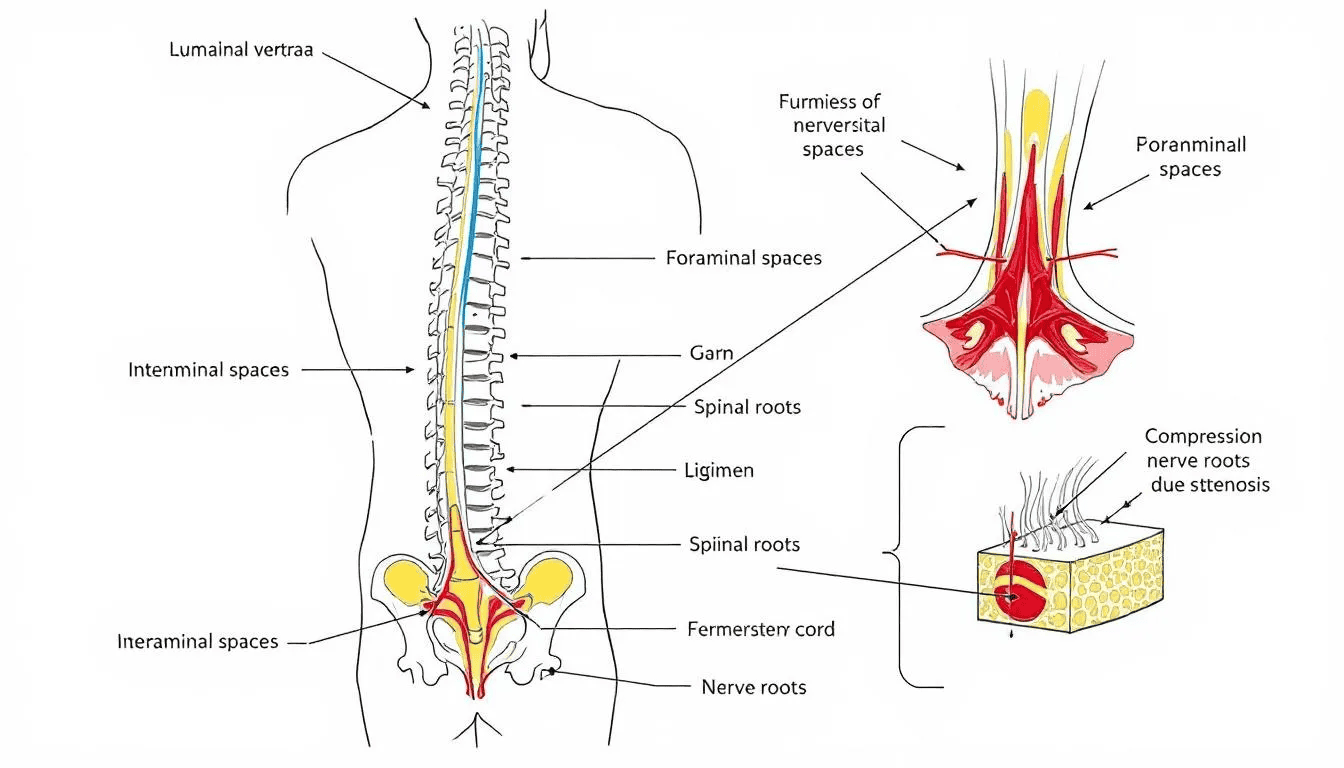
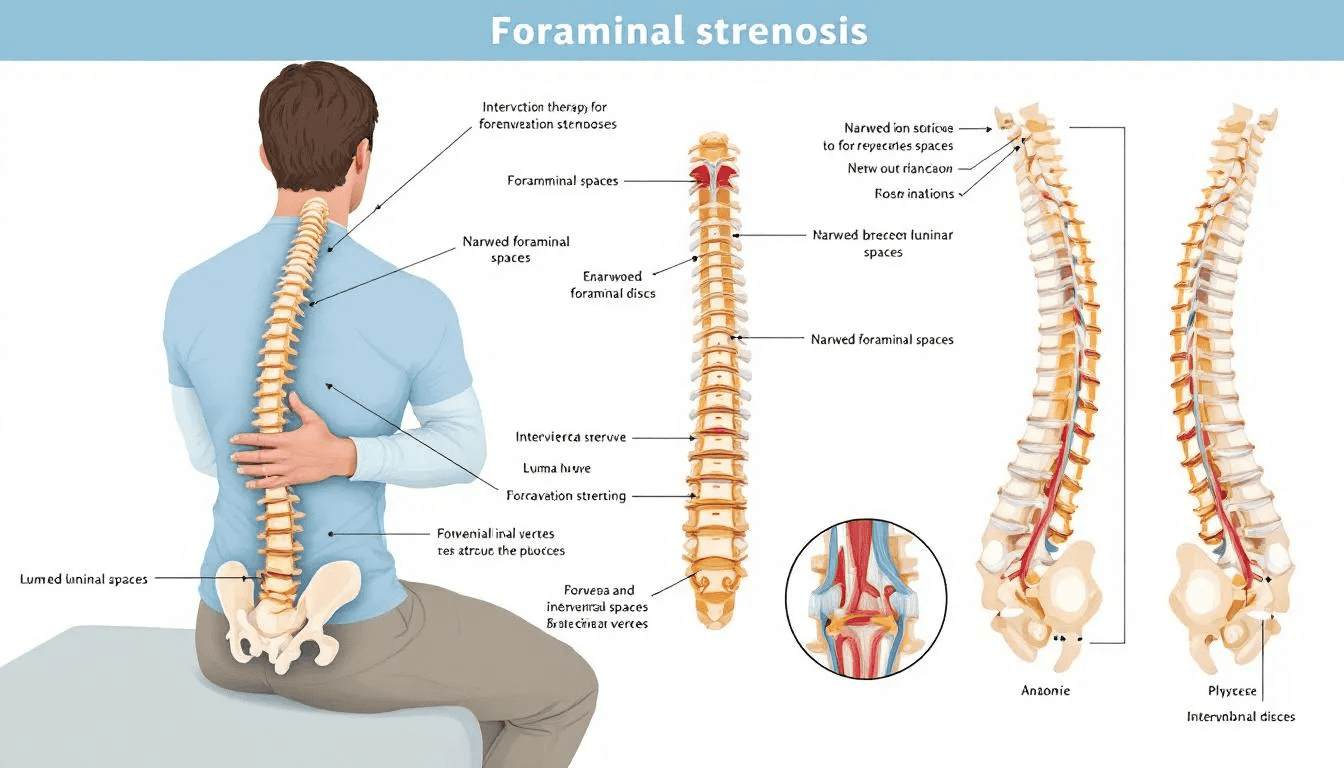
Foraminal stenosis is a spinal condition that occurs when the openings in the spinal canal, known as foramina, become narrowed. These foramina are crucial passageways that allow spinal nerves to exit the spinal cord and travel to other parts of the body. When these spaces become constricted, the spinal nerves can become compressed or irritated, leading to a variety of symptoms such as pain, numbness, tingling, and muscle weakness.
This narrowing can develop in any region of the spine, but it most commonly affects the cervical spine (neck) and lumbar spine (lower back). Cervical foraminal stenosis refers to narrowing in the neck area, while lumbar foraminal stenosis occurs in the lower back. Both types can significantly impact daily life, as the affected nerves are responsible for sensation and movement in the arms, legs, and other areas.
Understanding foraminal stenosis is essential for anyone experiencing unexplained pain or neurological symptoms. By learning about the causes, symptoms, and available treatments, individuals can take proactive steps to manage their spinal health and seek appropriate care when needed.
Key Takeaways
- Foraminal stenosis can affect individuals of all ages, with older adults and women being most susceptible due to degenerative spinal changes.
- Cervical and lumbar foraminal stenosis are the two main types, each presenting distinct symptoms and requiring targeted treatment approaches.
- Long-term management of foraminal stenosis involves lifestyle changes, physical therapy, and awareness of urgent symptoms that necessitate immediate medical attention.
Who Is Affected by Foraminal Stenosis?
Foraminal stenosis doesn’t discriminate; it can affect a wide range of people, although certain groups are more susceptible. Degenerative changes in the spine, often related to aging, are a significant contributor to foraminal stenosis in older adults. Foraminal stenosis affects both men and women but is more common in older adults, particularly those over 50. As we age, the disc degenerates in our spine can wear down, leading to conditions like foraminal stenosis. However, age isn’t the only factor at play here.
Interestingly, women are reported to be more frequently affected by cervical foraminal stenosis compared to men. The narrowing of the intervertebral foramina in the cervical spine typically develops as a part of the aging process in people over age 50. This disparity highlights the importance of understanding gender-specific health issues and the need for targeted medical interventions. Knowing that women are more prone to this condition can help in early diagnosis and treatment, potentially reducing the severity of symptoms.
Younger individuals aren’t entirely off the hook either. They can experience foraminal stenosis due to congenital abnormalities or herniated discs. Congenital factors, such as a naturally narrow spinal canal, can predispose someone to cervical foraminal stenosis from birth. Moreover, individuals with a family history of spinal disorders may have a higher susceptibility to developing foraminal stenosis. These genetic predispositions underline the need for vigilance and regular check-ups, especially if spinal issues run in the family. Reviewing a patient’s medical history is an important step in assessing risk and supporting early detection of foraminal stenosis.
Understanding who is affected by foraminal stenosis helps in early detection and proactive management. Recognizing the risk factors and being aware of family history allows for proactive monitoring and management of the condition before it becomes debilitating.
Types of Foraminal Stenosis
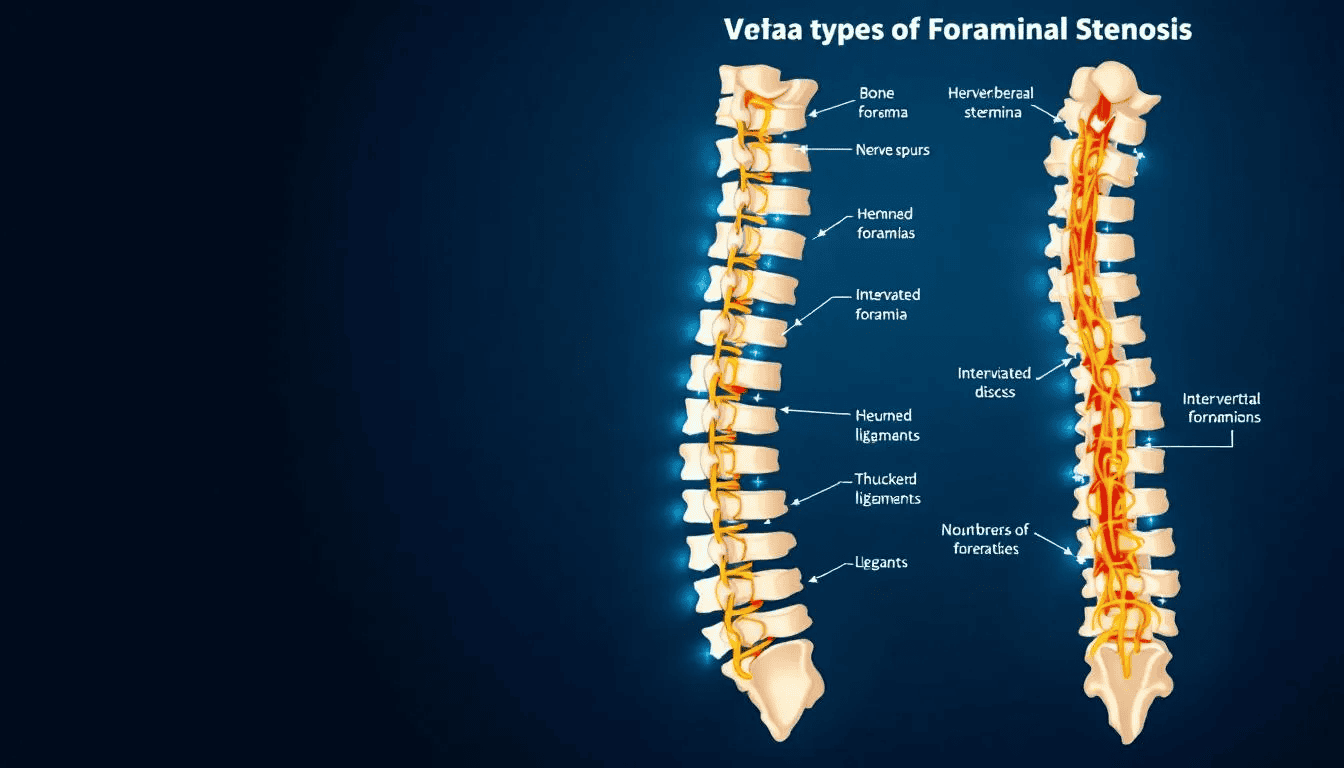
Foraminal stenosis manifests in various forms based on the affected spinal region. The two most prevalent types are cervical and lumbar foraminal stenosis, each with unique causes, symptoms, and treatment options. Thoracic foraminal stenosis is the least common type and occurs in the thoracic spine, which is located in the upper back area.
Cervical foraminal stenosis affects the neck region, while lumbar foraminal stenosis impacts the lower back. These distinctions are vital for accurate diagnosis and effective treatment. Next, we explore the distinct characteristics and effects of these two main types on the body.
Cervical Foraminal Stenosis
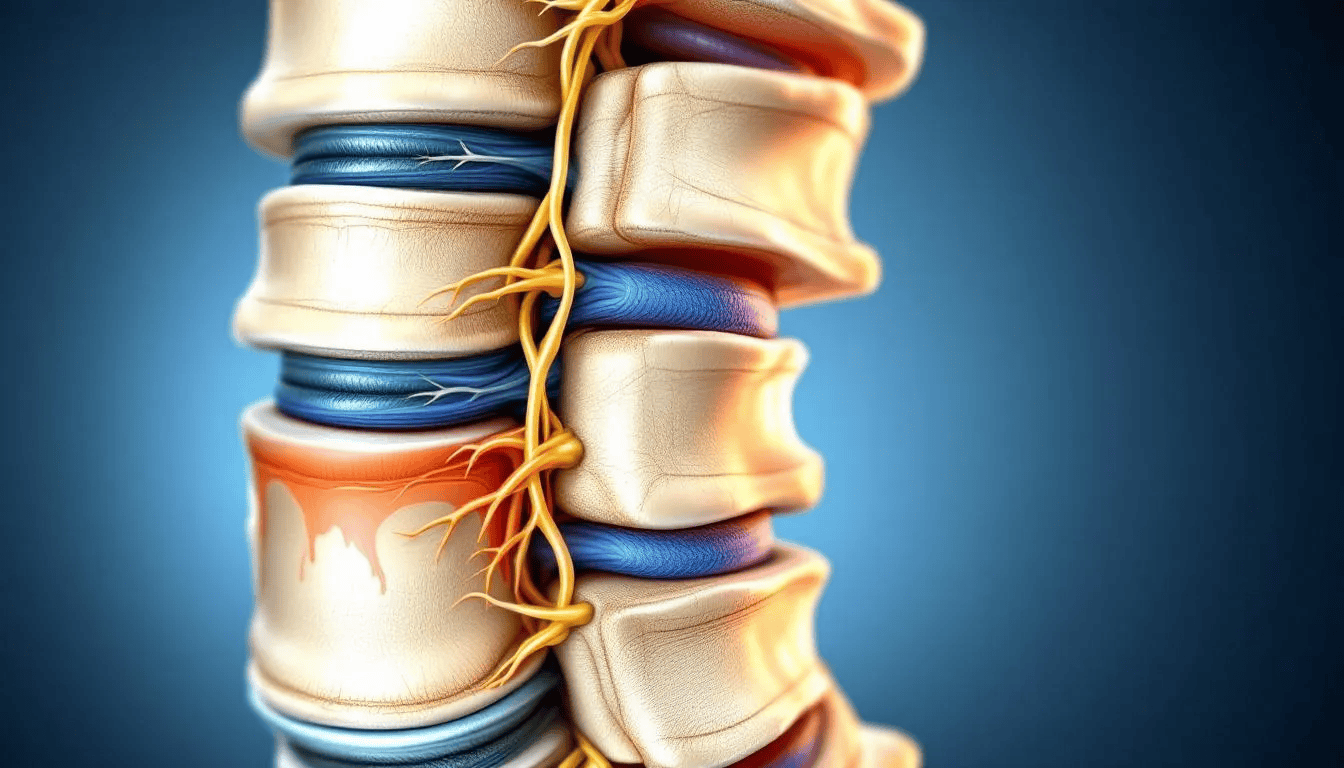
Cervical foraminal stenosis occurs in the neck region. It specifically affects the cervical spine and the cervical vertebrae. This condition is often caused by aging, disc degeneration, and the formation of bone spurs. Changes or damage to blood vessels can also reduce nourishment to the spinal discs, contributing to cervical disc degeneration and foraminal stenosis. These factors contribute to the narrowing of the foraminal spaces, which in turn narrowing puts pressure on the spinal nerve roots. The result is often significant discomfort and a range of other symptoms, including foraminal stenosis causes, neural foraminal stenosis, and cervical stenosis.
Common causes also include congenital factors and herniated disc. People born with a narrower spinal canal or those who experience disc herniation are at a higher risk of developing cervical foraminal stenosis. Additionally, spinal conditions like degenerative disc disease frequently accompany cervical foraminal stenosis, exacerbating the symptoms.
Symptoms of cervical foraminal stenosis can vary but often include neck pain, tingling, and numbness in the arms. The pressure on the spinal nerve roots can lead to nerve root compression and nerve compression, causing pain that can radiate through the shoulders and arms. Recognizing these symptoms aids in early diagnosis and treatment, helping to prevent the condition from worsening.
Lumbar Foraminal Stenosis
Lumbar foraminal stenosis occurs in the lower back, which is the most prevalent area for foraminal stenosis to occur. This condition can develop with or without central spinal stenosis, adding complexity to its diagnosis and treatment. Grasping the specific characteristics of lumbar foraminal stenosis is vital for effective management.
Symptoms of lumbar foraminal stenosis often include:
- Pain in the lower back, which can radiate down the legs
- Pain that is usually exacerbated by activities like standing or walking
- Pain that may improve when sitting
- Weakness or numbness in the legs due to involvement of nerve roots in the lower spine
Like cervical foraminal stenosis, lumbar foraminal stenosis can be caused by degenerative changes, disc herniation, and the formation of bone spurs. Thickened ligaments encroach on nerve pathways and are a contributing factor to foraminal stenosis. These conditions lead to the narrowing of the spinal canal and foraminal spaces, putting pressure on the spinal nerves. Cervical foraminal stenosis can lead to complications such as the loss of bladder and bowel control or partial or full leg paralysis. Early diagnosis and targeted treatment can help alleviate symptoms and improve quality of life for those affected by lumbar foraminal stenosis.
Common Foraminal Stenosis Symptoms
The symptoms of foraminal stenosis can range from mild discomfort to severe pain, significantly impacting daily life. Symptoms can vary in intensity from a mild annoyance to severe or debilitating. Common spinal stenosis symptoms include:
- Pain
- Tingling
- Numbness
- Muscle weakness These symptoms can vary in intensity and may affect different parts of the body depending on the location of the stenosis.
For instance, cervical foraminal stenosis symptoms often include neck pain, which can radiate to the shoulder blades and arms. When the stenosis occurs at the C3-C4 level, the pain is typically localized in the neck, while involvement of the C5-C6-C7 levels can lead to arm pain.
Lumbar foraminal stenosis symptoms, on the other hand, often manifest as lower back pain that radiates down to leg pain, causing discomfort and mobility issues.
It’s important to note that symptoms of foraminal stenosis may come and go but can also develop into chronic issues. Some patients experience shooting pain through their extremities, which can be particularly debilitating. Recognizing these symptoms early and seeking medical advice can help manage the condition effectively and prevent it from worsening.
Diagnostic Methods for Foraminal Stenosis
Diagnosing foraminal stenosis diagnosed involves a combination of symptom assessment, physical exams, and imaging techniques. Diagnostic tests are essential for identifying and confirming cervical foraminal stenosis, and for guiding treatment decisions. Not everyone with cervical foraminal stenosis will show symptoms; some can have narrowing visible on imaging without any associated pain or neurological deficits. The presence and location of symptoms can provide valuable clues for identifying the specific area of stenosis. For example, symptoms from lumbar foraminal stenosis often worsen when standing and improve when sitting.
A physical exam is usually conducted to assess muscle strength, reflexes, and range of motion, helping to pinpoint the affected area. Imaging techniques like X-rays, MRI, and CT scans are crucial for a definitive diagnosis. X-rays can reveal changes in bone structure that contribute to foraminal narrowing, while MRI scans provide detailed images of both hard and soft tissues, making it easier to evaluate the extent of the stenosis.
In cases where magnetic resonance imaging is not suitable, a CT scan can offer 3D images of the spine, providing a clear view of the affected areas. A CT myelogram, which involves injecting contrast dye, can enhance the visualization of spinal structures, making it easier to identify the precise location and severity of the stenosis. These advanced techniques, including computed tomography, are essential for developing an effective treatment plan. Other diagnostic tests may be used to confirm nerve compression or narrowing in the cervical spine, especially when planning appropriate treatment or surgical interventions.
Non-Surgical Treatments for Foraminal Stenosis
Initial treatments for foraminal stenosis often focus on relieving pain relief and improving function without requiring non surgical treatment. Your doctor will likely start with conservative (nonsurgical) treatment options. These treatments include:
- Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen to reduce inflammation and pain
- Physical therapy
- Specific exercises
- Heat or ice therapy to provide relief while treating foraminal stenosis
For cervical foraminal stenosis, common non-surgical treatments include:
- NSAIDs
- Oral steroids
- Muscle relaxers, which may be prescribed to relieve spasms and tension, aiding in the management of pain associated with foraminal narrowing
- Pain relievers
- Physical therapy
- Steroid injections, such as epidural steroid injections that deliver pain-relieving medication directly into the epidural space around the spinal cord, providing targeted relief.
Physical therapy aims to improve mobility and strength by guiding patients through specific exercises tailored to alleviate symptoms of foraminal stenosis. These non-surgical treatments are often effective in managing mild to moderate symptoms, helping patients maintain a good quality of life without the need for surgical intervention.
Surgical Options for Severe Foraminal Stenosis
In cases where non-surgical treatments fail to provide relief, surgery may be recommended. After foraminal stenosis surgery, you may need to rest for a few days and allow the surgical site to heal. Surgical options for foraminal stenosis include:
- Foraminotomy: involves removing bone or tissue to enlarge the foraminal space and relieve pressure on the spinal nerves.
- Traditional open surgery
- Minimally invasive surgery.
Minimally invasive surgery offers several advantages, such as smaller incisions, reduced muscle damage, and shorter recovery times. These procedures are often preferred for their effectiveness and quicker recovery. Lumbar foraminal stenosis frequently coexists with conditions affecting the central spinal canal, making it essential to address all contributing factors during spinal surgery.
Choosing the right surgical option depends on the severity of the stenosis, the patient’s overall health, and the specific symptoms. Consulting with a spine specialist can help determine the most appropriate spine surgery intervention, ensuring the best possible outcome for patients with severe foraminal stenosis.
Prevention of Foraminal Stenosis
While some risk factors for foraminal stenosis, such as age and genetics, cannot be changed, there are several proactive steps you can take to help protect your spine and reduce your risk of developing this condition. Regular physical therapy and exercise play a key role in strengthening the muscles that support the spine, improving flexibility, and minimizing the likelihood of spinal injuries or degenerative changes that can lead to foraminal narrowing.
Practicing proper lifting techniques and maintaining good posture throughout daily activities can significantly reduce strain on the spine, helping to prevent issues like herniated discs and bone spurs—two common causes of nerve pain and leg pain associated with foraminal stenosis. Managing risk factors such as high blood pressure, excess weight, and smoking is also important, as these can contribute to poor spinal health and increase the risk of developing symptoms.
A balanced diet rich in nutrients supports bone and nerve health, while regular check-ups with your healthcare provider can help catch early signs of spinal problems before they become severe. In some cases, your doctor may recommend nonsteroidal anti-inflammatory drugs (NSAIDs) or muscle relaxers to manage mild symptoms and prevent further degeneration.
By staying active, making healthy lifestyle choices, and being mindful of your spine’s well-being, you can help prevent the onset of foraminal stenosis and reduce the risk of experiencing neck pain, nerve pain, or other related symptoms. Taking these steps not only supports your spinal health but also contributes to your overall quality of life.
Managing Foraminal Stenosis Long-Term
Managing foraminal stenosis long-term involves: Pain and nerve-related issues are often easier to treat early on.
- A combination of lifestyle changes, physical therapy, and ongoing medical care.
- Addressing lifestyle factors like obesity and sedentary behavior, which can increase the risk of developing foraminal stenosis.
- Maintaining a healthy weight, as excess body weight can exacerbate pressure on the spine.
Good posture is crucial for reducing strain on the spine and alleviating discomfort caused by foraminal stenosis. Engaging in low-impact exercises, such as swimming and walking, can help support spinal health and alleviate symptoms. Flexion exercises, which involve bending the spine forward, can increase spinal canal space and relieve pressure on nerves.
Working with a physical therapist can help develop a personalized exercise program to improve strength and flexibility. Avoiding high-impact exercises is advisable, as they can worsen symptoms and create additional strain on the spine. Adopting these long-term management strategies helps individuals maintain a good quality of life and prevent the condition from progressing.
When to Seek Immediate Medical Attention
While many symptoms of foraminal stenosis can be managed with non-surgical treatments, certain symptoms warrant immediate medical attention. Urgent symptoms often include:
- Severe pain
- Significant muscle weakness
- Neurological deficits
- Acute neck or back pain
- Inability to control movement in limbs
- Sudden changes in bladder or bowel function
These are clear indicators that immediate medical care is needed.
Ignoring these symptoms can lead to permanent nerve pain or loss of function, significantly affecting daily activities. Prompt medical attention can help alleviate symptoms and prevent further complications, improving long-term outcomes. If you or someone you know experiences these severe cases or a pinched nerve, seeking immediate medical care is crucial. Severe neural foraminal stenosis can lead to complications such as loss of bladder and bowel control or paralysis, though this is rare.
Summary
Foraminal stenosis can have a significant impact on quality of life, but understanding its symptoms, causes, and treatments can empower individuals to manage the condition effectively. From recognizing who is at risk to understanding the different types and symptoms, early diagnosis and targeted treatment can make a world of difference. Interestingly, most people who have foraminal stenosis don’t know they have it because most cases don’t cause symptoms.
Whether through non-surgical treatments or, in severe cases, surgical interventions, there are options available to help manage and alleviate the symptoms of foraminal stenosis. By adopting long-term management strategies and knowing when to seek immediate medical attention, individuals can take proactive steps to maintain their spinal health and overall well-being.
Frequently Asked Questions
What are the primary causes of foraminal stenosis?
The primary causes of foraminal stenosis are degenerative changes associated with aging, disc degeneration, bone spur formation, congenital conditions, and herniated discs. Understanding these factors is crucial for effective management and treatment.
What are the common symptoms of cervical foraminal stenosis?
Cervical foraminal stenosis commonly presents with neck pain, tingling, numbness, and muscle weakness, often radiating to the shoulders and arms due to nerve root compression. It is important to consult a healthcare professional for appropriate evaluation and treatment.
How is foraminal stenosis diagnosed?
Foraminal stenosis is diagnosed by evaluating symptoms, conducting physical examinations, and utilizing imaging techniques like X-rays, MRI, and CT scans to assess the narrowing of foraminal spaces and nerve compression. These diagnostic approaches provide a comprehensive understanding of the condition.
What non-surgical treatments are available for foraminal stenosis?
Non-surgical treatments for foraminal stenosis include NSAIDs, physical therapy, specific exercises, heat or ice therapy, muscle relaxers, oral steroids, pain relievers, and epidural steroid injections. These options are designed to alleviate pain and enhance mobility effectively.
When should I seek immediate medical attention for foraminal stenosis?
Seek immediate medical attention if you experience severe pain, significant muscle weakness, neurological deficits, acute neck or back pain, loss of limb movement, or sudden changes in bladder or bowel function, as these symptoms may indicate severe nerve compression requiring urgent care.











